If you work in healthcare, you likely have been the recipient of a call from a donor looking for help.
The donor might be asking for help scheduling an appointment (often seeking a slot sooner than what the donor could get on their own), securing a private room, assisting a friend or family member in a medical crisis, or smoothing out a challenging healthcare experience. These requests raise a host of ethical and logistical challenges. Forces in society and the healthcare industry are shaping contemporary views of facilitated access programs. From healthcare equity to labor shortages to burnout, difficult times put more pressure on philanthropy to deliver.
Facilitated Access Defined
Facilitated access is a means of providing, either formally or informally, assistance to donors and often their families or associates with the healthcare experience. Depending on the institution, it may involve scheduling appointments; coordinating appointments or hospital stays; assisting with healthcare navigation; procuring amenities like blankets or personal care items; gaining access to physicians, private rooms, separate waiting rooms, or upgraded spaces; and more. Some institutions have formal programs, with websites and extensive staff that may include physicians, nurses, or navigators. Others choose not to promote the services they offer and only quietly and discretely disclose services to qualifying donors. And still others just handle requests without any formal system, with development and clinical teams together figuring out the situation each time.
Facilitated access programs differ from concierge medicine programs, which provide personalized attention, fast responses, and high-touch care to patients willing to pay a fee for a higher level of service. Often, facilitated access and concierge medicine programs have overlapping audiences and participants, but facilitated access programs are based on philanthropic support, not a fee for service.
The Challenges We Face
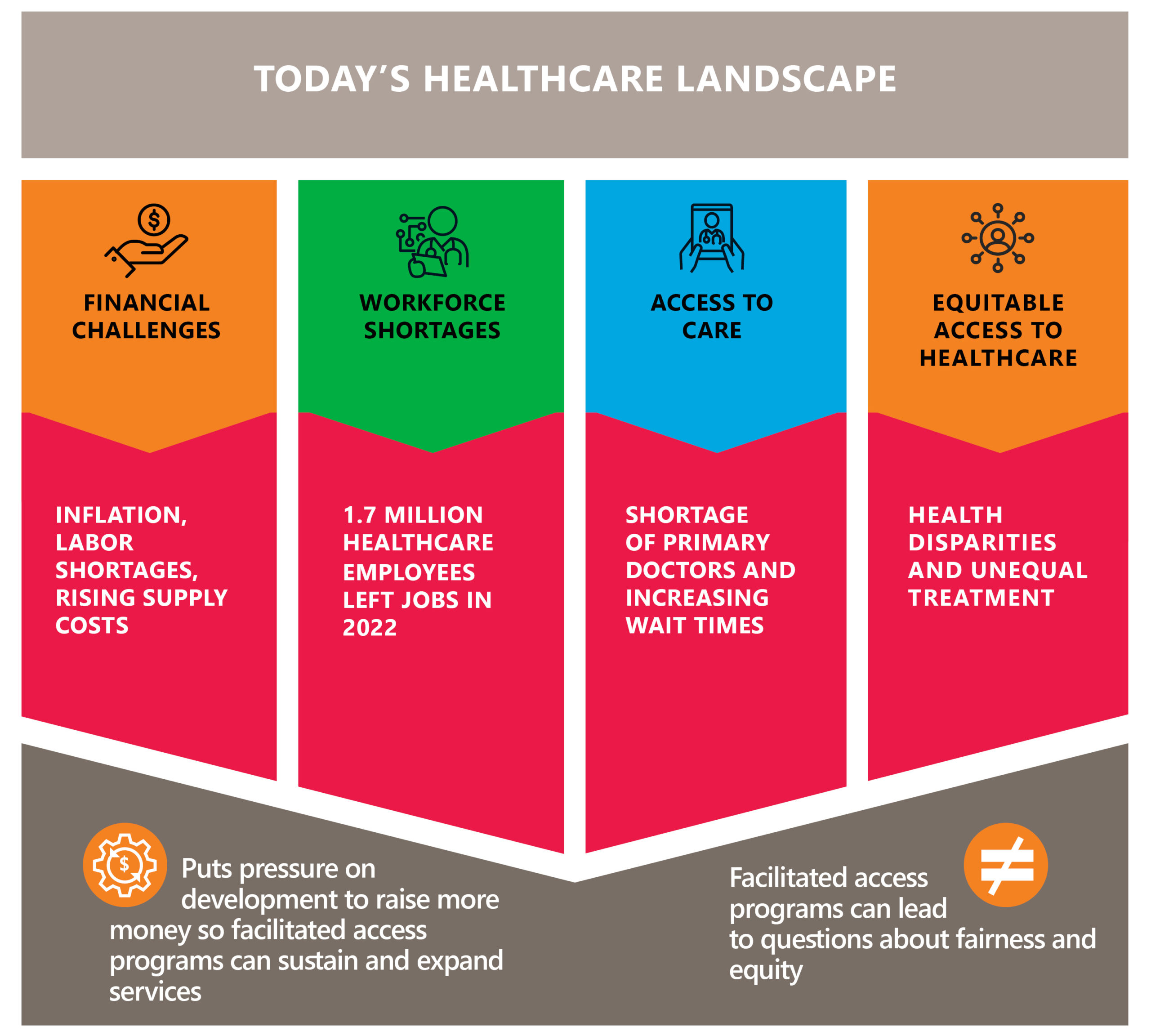
In today’s healthcare landscape, there are many pressures and issues influencing the industry.
- The global COVID-19 pandemic laid bare issues around the equitable access to healthcare. During the early days of COVID-19 vaccines, several facilitated access programs faced public outrage for offering vaccines to donors ahead of other patients or employees.
- Across the country, patients are challenged to access care. Growing shortages of primary care doctors and increasing wait times for specialists leave patients frustrated with healthcare systems they feel are not delivering the care they need, when they need it.
- Workforce shortages add to challenges in healthcare access. In 2022, over 1.7 million healthcare employees left their jobs, about 3% of the healthcare workforce each month.
- Healthcare institutions face the most difficult financial situation since the start of the COVID-19 pandemic. The combination of inflation, labor shortages, and rising supply costs squeeze hospital margins. In a report by Kaufman Hall for the AHA, it is projected that at best half of the hospitals in the United States will end the year in the red.
How do all of these challenges relate to facilitated access programs? Financial challenges put pressure on development teams to raise more money to sustain and expand services. But offering facilitated access programs can lead to questions about fairness and equity. Challenging times, indeed.
Determining Your Approach
Donor requests for assistance, combined with the societal and structural challenges in healthcare, leave facilitated access programs in a fraught position.
On the one hand, healthcare institutions recognize that donors are members of the institution’s family. Philanthropy often provides the margin of excellence in hospitals and medical centers, and gifts that support patient care, facilities, research, and medical education benefit all patients. Creating a formal program helps appropriately manage healthcare requests from donors. Gift officers may find these requests problematic or even uncomfortable, due to the obvious HIPAA and privacy concerns and distractions from their other fundraising work.
On the other hand, the ethical and clinical concerns surrounding facilitated access deserve consideration. Some clinicians and community members express fear that these programs allow donors to jump ahead of other patients or get better medical care, even if institutions construct their programs to expressly avoid such inequities. With many clinicians already feeling stretched to care for the patients on their schedule, a request to add one more may feel overwhelming, only furthering the stress that leads to burnout.
The reality is that the requests from donors are unlikely to ever stop, so a thoughtful approach that is right for your institution and your donors is a smart move. If you are thinking about initiating a facilitated access program, or you are reexamining an existing one, start by focusing on three questions:
#1 What are the risks and benefits of a facilitated services program for your institution?
The best approach to facilitated services will vary by institution based on culture and donor base. There is no “one-size-fits-all” approach for facilitated access programs. At this initial stage, talking with institutional leaders in the legal, public relations, operational, governance, and clinical spheres may help you uncover important cultural considerations and insights. In your dialogue with leaders, the following list of questions related to benefits and risks may help you guide the key points in the conversation.
Possible benefits:
- Does a defined process for handling such requests provide a better experience for our benefactors?
- Does a defined process mitigate risks or distractions for development staff?
- Does a program help us steward our donors, inspiring additional philanthropy?
- Could this program help our organization learn how to provide a better healthcare experience for all?
Possible risks:
- Could a facilitated access program initiate or exacerbate real or perceived issues in health access and equity?
- Could a program frustrate or anger clinical and other staff who may already be stretched thin?
- How might the community react to a facilitated access program?
- Could we find the budget and staffing for such a program?
#2 What kind of program fits our institutional culture?
Taking your risks and benefits into account, evaluate what kind of program fits your culture. Consider four key areas:
Services Offered
From scheduling visits and private rooms to helicopter transfers and private nurses, donors have been known to ask for a wide range of things that make their healthcare experience easier for them. Your institution should review the kinds of requests you’ve received and use that as a starting point for a conversation around the types of services your institution might offer.
Role of Development
Given the close relationships development officers form with donors, they naturally receive healthcare requests from their patient donors. This can put those development officers in awkward situations, and given privacy and HIPAA concerns, some healthcare institutions are reevaluating the role development plays in the facilitated access program. Based on your institution’s comfort level, the development office could exclusively manage the facilitated access program, or, more conservatively, your organization may choose to direct all donor requests to staff in a clinical space or even an executive office.
Target Constituency
How big of a program do you want or can handle successfully? Take a careful look at your data and analyze how many donors or volunteers could have access to a program. Consider how expansive your program will be. Does it include the donor and their immediate family? Extended family? Business associates? Once you set your boundaries, how will you handle requests that fall outside of that? Or, is there a phone number that is passed along to donors who meet criteria but is available to anyone else who has the number? Careful planning upfront for the size and scope of your program can avoid an overwhelming situation later.
To Promote the Program … or Not
Your knowledge of your institution, community, and local culture should inform your approach to publicizing your facilitated access program. Should you promote your facilitated access program through websites, brochures, or posters in the hopes of attracting new donors to the qualifying level of support? Or given the public relations risks, is it better to share information only with those who qualify and forego public-facing promotion and the scrutiny that comes along with it?
#3 How do you successfully implement your facilitated access concept?
After you have given careful thought to your cultural context and the appropriate program design, it’s time to call on your key partners in operations, clinical care, nursing, and other areas to help you operationalize your concept. Engaging these partners from the beginning of the implementation phase will help you gain their trust and support, important because each play a role in delivering care or access. A solid, collaborative partnership between development and these operational and clinical partners forms the foundation critical to launching and sustaining any facilitated access program. Together, you should consider several important factors before launching:
Process
Determine step-by-step how a request would be handled, even using some past requests as examples. Plan for the unexpected or rarer scenarios when a request comes in on a holiday or when a key staff member is on vacation. Together with your partners, test your model until you are confident you have all of the plans—and backup plans—to have your facilitated access program run smoothly.
Staffing
Whether your program involves staff within your development office or in other departments, now is the time to work on job descriptions for any new or modified roles. For all programs, but especially for programs that involve staff in multiple departments, ensure all roles fit the program design and that everyone involved has the same understanding of reporting lines, responsibilities, and expectations.
Budget
Closely tied to staffing is the budget, since your facilitated access program’s biggest expense is likely to be the staff. You may also have costs associated with marketing, space, or amenities to consider. To build a strong case for the investment in the facilitated access program, use your analysis of the benefits of such a program for your organization and donors.
Building on Your Culture
With the complex issues surrounding facilitated access, where do you begin an evaluation of a current program or the development of a new one? Always start with your institutional culture. Rooting your program in the culture and mission of your institution will help you design a program that finds the right balance of services provided by the right people.
Next, remember to tap into your team. Working collaboratively across the institution, your colleagues in clinical, operations, and administrative departments will help you evaluate the risks and opportunities presented in a facilitated access program and consider the options for designing your own. When you are ready to launch your program, their support and participation will be essential.
Lastly, consider starting small before scaling up. A time-limited pilot project could help you test the program design and gain valuable feedback—from donors and internal partners alike. Similarly, launching the program with a small group of close volunteers or donors allows you to ensure the program works smoothly before you roll it out to your full audience.
Once you’re grounded in your culture and working with clinical and development partners across your institution, you’ll be prepared the next time a donor calls asking for help.